General medicine case 5
This is an online e-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
Date of admission : 17/10/21
A 37 year old man who is farmer by occupation came to the OPD with the chief complaint of
1. Constipation since 1 day
2. Decreased urine output since 1 day
3. Vomitings since 1 day
4. Pain in abdomen since 4 days
History of present illness :
- The patient was apparently asymptomatic 5 days back when he observed pain in abdomen for which he took symptomatic treatment for two days in a local hospital.
- The condition subsided but recurred after a day along with constipation, decreased urine output and vomiting that was non bilious in nature.
History of past illness :
- The patient is not a known case of diabetes, hypertension, epilepsy, tuberculosis, asthma
Personal history :
- The patient has no loss of appetite
- He takes mixed diet
- No sleep disturbances
- The patient takes 90 -100 ml of alcohol daily and consumes non smoking form of tobacco daily since 20 years
Family history :
- There are no similar complaints in the family members
Treatment history :
- The patient has taken medications for abdominal pain
- He is not a known case of drug allergy.
General examination :
- Patient is conscious, coherent, cooperative at the time of joining
- No pallor
- No icterus
- No cyanosis
- No clubbing of fingers and toes
- No lymphadenopathy
- No pedal edema
Vitals : temperature - afebrile
Pulse rate - 94 bpm
Respiratory rate - 22 cycles per minute
BP - 140/90 mm Hg
Systemic examination :
CVS
Inspection - chest wall is bilaterally symmetrical
- No precordial bulge
- No visible pulsations, engorged veins, scars, sinuses
Palpation - JVP is normal
Auscultation - S1 and S2 heard
RESPIRATORY SYSTEM
- Position of trachea is central
- Bilateral air entry us normal
- Normal vesicular breath sounds heard
- No added sounds
PER ABDOMEN
- abdomen is tender
- bowel sounds heard
- no palpable mass or free fluid
CNS
- Patient is conscious
- Speech is present
- Reflexes are normal
Investigations :
Hemogram :
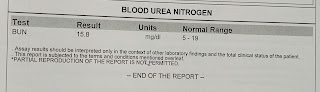
Blood urea nitrogen :
ECG :
Ultrasound report :







Comments
Post a Comment